The Peripheral nervous System
The brachial plexus consists of the anterior branches of the C5 to T1 spinal nerves on each side. These arise immediately after the exit of the spinal nerves from the vertebral column, course across the neck and behind the clavicle (collar-bone) to provide branches that give nerve supply to the different muscles of the upper limb and carry sensations from the different parts of the upper limb to the brain (via the spinal cord).
Injury to Brachial Plexus
There is a ray of hope for all accidents victims (mainly road accidents) whose limbs have been paralyzed due to internal nerve damage. We restore paralyzed limbs of accident victims to ensure partial movement of the affected part. Results depend on the severity of the injury and may vary from person to person.
Nerves can be internally damaged (or completely broken) without any visible external physical injury.
Total Paralysis
 Here, the patient is unable to move any portion of the upper limb (shoulder, elbow, wrist, fingers). Usually, shrugging of the shoulder is possible as this action requires use of the trapezius muscle, which receives nerve supply from the spinal accessory nerve. This nerve lies outside the brachial plexus and is usually spared in these accidents. If this flail situation persists for a month from the accident, it implies a severe injury to all five nerves of the brachial plexus at a very high level (in the neck close to the vertebral column).
Here, the patient is unable to move any portion of the upper limb (shoulder, elbow, wrist, fingers). Usually, shrugging of the shoulder is possible as this action requires use of the trapezius muscle, which receives nerve supply from the spinal accessory nerve. This nerve lies outside the brachial plexus and is usually spared in these accidents. If this flail situation persists for a month from the accident, it implies a severe injury to all five nerves of the brachial plexus at a very high level (in the neck close to the vertebral column).
This can be confirmed by performing a cervical myelogram (a test that involves injection of a dye into the spinal canal followed by an x-ray of the neck). Surgical reconstruction offers the only means for restoration of some selected muscles in such paralysed upper limbs.
Incomplete Paralysis
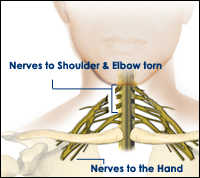 In such cases, the nerves to the hand (C8 and T1) are usually spared (may be partially stretched or torn) and the patient can bend the fingers, thumb and wrist. Sometimes, the patient retains the ability to straighten the wrist, fingers and, even, the elbow. However, there is no strength in the muscles that move the shouler or bend the elbow. A diagnosis of irrecoverable injury is usually made if the situation persists for two months. It is confirmed with the help of a cervical myelogram and EMG testing of the paralysed muscles. Surgery involves nerve grafting or nerve transfers for restoration of the lost shoulder and elbow functions.
In such cases, the nerves to the hand (C8 and T1) are usually spared (may be partially stretched or torn) and the patient can bend the fingers, thumb and wrist. Sometimes, the patient retains the ability to straighten the wrist, fingers and, even, the elbow. However, there is no strength in the muscles that move the shouler or bend the elbow. A diagnosis of irrecoverable injury is usually made if the situation persists for two months. It is confirmed with the help of a cervical myelogram and EMG testing of the paralysed muscles. Surgery involves nerve grafting or nerve transfers for restoration of the lost shoulder and elbow functions.
Total Paralysis
Surgery in brachial plexus injuries involves re-establishment of the connection between the central nervous system (brain and spinal cord) and the target muscles in the upper limb. A source of growing nerve fibers (a stump of a spinal nerve) is an essential pre-requisite for this purpose. The gap between this nerve end and the specific target nerves is bridged by placing nerve graft cables. These cables are derived from cutaneous nerves (those supplying sensation to the skin) from the legs. This procedure does not produce any deficit in the legs. The cables are stitched at each end using fine nylon threads under the operating microscope. The nerve grafts serve as pathways to direct the growth of the nerve fibers towards the target nerves.
Incomplete Paralysis
In 25-30% of patients, only the upper roots of the brachial plexus (C56 or C567) are affected while the lower roots are partly injured or spared. In such cases, the patient loses power in the shoulder and the elbow while the movements of bending and straightening of the fingers are retained. Function in the shoulder and elbow can be restored in a large percentage of cases (80%) by means of nerve transfers or nerve grafting from available root stumps in the neck. Hence, such patients are more likely to regain almost full use of the affected upper limb.
The retained function in the lower roots (C8T1 and ulnar nerve) implies that an additional donor of growing nerve ends is available. Professor Christophe Oberlin of Paris showed that 10% of fibers of the ulnar nerve could be safely transferred to the biceps in the arm (Journal of Hand Surgery 1994) without producing any deficit in the hand. The biceps function is regained rapidly (4-6 months) in 80% of suitable patients.
As a result, other nerve transfers (spinal accessory and intercostal nerves) can be deployed for restoration of shoulder function and elbow extension. In such patients with retained hand functions, diverting the intercostal nerves to the triceps muscle can facilitate reaching out for objects.